
Continuing Competence Program
Peer Dialogue Reflection Example Submissions
Competence is the combination of:
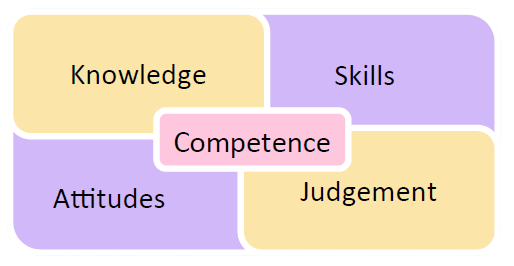
The sample reflections all detail how the regulated member’s knowledge, skills, attitudes and/or judgement were positively impacted by the continuing education activities they completed.
Note that in these reflections, the members provided specific information about knowledge gained or changes to practice (i.e., changes to their skills, attitudes, or judgement) that occurred, and included:
- Practice areas or diagnoses,
- Population groups, including client age ranges, and/or
- Specific clinical or nonclinical skills that were impacted.
Note also that these reflections focused on the impact(s) to the members’ own competence, rather than the competence of the peer with whom they had the discussion.
Audiology Reflection Example:
SLP Reflection Examples:
Non-clinical Examples:
